Why Seniors Get Joint Pain and the Best Ways to Manage It

Joint pain affects millions of seniors, making everyday activities like climbing stairs or opening jars feel challenging. If you’re over 50 and dealing with stiff, aching joints, you’re not alone—and there are proven ways to find relief.
This guide is designed for older adults experiencing joint discomfort and their caregivers who want practical solutions. You’ll discover why our bodies develop joint pain as we age and learn about the most common types that affect seniors. We’ll also explore lifestyle changes that can reduce your discomfort and cover both medical treatments and natural remedies that work well together to manage pain effectively.
Understanding Why Aging Bodies Develop Joint Pain
Natural cartilage breakdown and wear over time
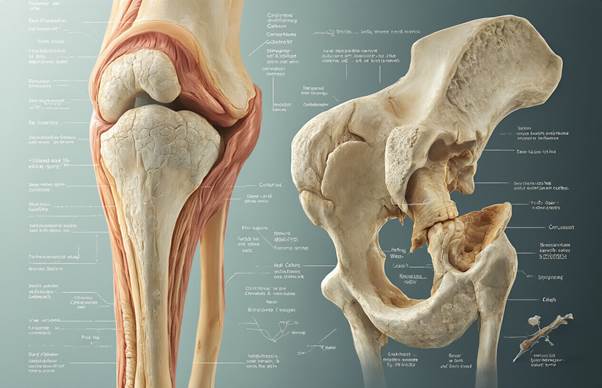
Cartilage serves as the smooth, rubbery cushion that covers the ends of bones in your joints, allowing them to glide effortlessly against each other. Think of it as nature’s shock absorber – when you’re young, this tissue is thick, resilient, and perfectly designed to handle the daily demands of movement.
As the years pass, cartilage begins to thin and deteriorate through normal wear and tear. Unlike other tissues in your body, cartilage has no blood supply, which means it can’t repair itself effectively once damage occurs. This creates a gradual breakdown cycle where small tears and rough spots develop on the cartilage surface.
The deterioration process happens slowly, often taking decades before you notice symptoms. Activities that once felt effortless – climbing stairs, gardening, or even getting out of bed – can become uncomfortable as the cartilage loses its protective qualities. Weight-bearing joints like knees, hips, and ankles typically show the most dramatic changes since they handle the greatest mechanical stress throughout life.
Reduced synovial fluid production affects joint lubrication
Your joints contain a special fluid called synovial fluid that acts like high-quality motor oil for your body’s moving parts. This clear, viscous liquid lubricates joint surfaces, reduces friction, and delivers nutrients to cartilage cells.
Aging bodies produce less synovial fluid, and the fluid that remains becomes thinner and less effective at its job. This reduction in both quantity and quality means your joints operate with less lubrication than they need for smooth movement.
Without adequate synovial fluid, joints become stiff, especially after periods of inactivity. You might notice this most clearly in the morning when your joints feel “creaky” after a night’s rest, or after sitting for extended periods. The decreased lubrication also means that everyday movements create more friction between joint surfaces, which can accelerate cartilage wear and increase discomfort.
Muscle mass loss creates additional joint stress
Starting around age 30, people naturally lose muscle mass at a rate of 3-8% per decade, with this loss accelerating after age 60. This condition, called sarcopenia, directly impacts joint health in significant ways.
Strong muscles act as natural shock absorbers and stabilizers for your joints. When muscle mass decreases, joints must handle more stress during daily activities. Your knee muscles, for instance, help absorb the impact when you walk or climb stairs – weaker muscles mean your knee joints bear more of that force directly.
Muscle weakness also affects your balance and movement patterns. When muscles can’t provide adequate support, you might unconsciously change how you walk, stand, or move to compensate. These altered movement patterns can place unusual stress on joints, creating new pressure points and accelerating wear in areas that weren’t designed to handle such forces.
Hormonal changes accelerate joint deterioration
Hormones play a crucial role in maintaining healthy joint tissues, and aging brings significant changes to hormone production that directly affect joint health.
Estrogen decline during menopause particularly impacts women’s joint health. This hormone helps maintain cartilage and bone density, so when estrogen levels drop, cartilage becomes more vulnerable to breakdown. Many women notice increased joint stiffness and discomfort during and after menopause, especially in their hands, knees, and spine.
Growth hormone production also decreases with age, affecting the body’s ability to repair and maintain joint tissues. Lower growth hormone levels mean slower healing of micro-injuries that occur in joints during normal use.
Testosterone levels in men similarly decline over time, affecting muscle mass maintenance and bone strength. These hormonal shifts create a perfect storm where joints receive less protection from surrounding tissues while simultaneously becoming more susceptible to damage and less capable of self-repair.
Common Types of Joint Pain That Affect Seniors

Osteoarthritis symptoms and affected areas
The most widespread joint condition among seniors, osteoarthritis strikes when cartilage breaks down over years of use. You’ll typically feel a deep, aching pain that gets worse with activity and improves with rest. Morning stiffness lasts less than 30 minutes, unlike other forms of arthritis.
The knees bear the brunt of this condition, causing pain when climbing stairs, getting up from chairs, or walking long distances. Hip osteoarthritis creates discomfort in the groin area that sometimes radiates down the thigh. Your hands might develop those telltale bony bumps called Heberden’s nodes at the fingertips or Bouchard’s nodes at the middle joints.
Spine involvement brings lower back pain and neck stiffness. The pain often feels like a grinding sensation, and you might hear actual creaking sounds when moving affected joints. Weather changes can make symptoms flare up, leaving many seniors predicting storms better than meteorologists.
Rheumatoid arthritis warning signs and progression
Rheumatoid arthritis announces itself differently than osteoarthritis. Morning stiffness stretches beyond an hour, and your joints feel warm and swollen rather than just achy. This autoimmune condition attacks the lining of joints, creating inflammation that spreads symmetrically across your body.
Small joints in your hands and feet usually show symptoms first. You might notice your knuckles looking puffy or your wedding ring feeling tight. Fatigue hits hard with rheumatoid arthritis – not just tired, but completely drained like you’re fighting off the flu.
The condition progresses in flares and remissions. During active periods, you might run a low-grade fever and lose your appetite. Joints become tender to touch, and simple tasks like opening jars or buttoning shirts become challenging. Without proper treatment, joint deformity can develop as the disease attacks cartilage, bones, and surrounding tissues.
Bursitis pain patterns and triggers
Bursitis targets the small, fluid-filled sacs that cushion your joints. The pain feels sharp and localized, quite different from the broader aching of arthritis. Common trouble spots include shoulders, hips, elbows, and knees.
Shoulder bursitis creates pain when reaching overhead or sleeping on the affected side. Hip bursitis hurts most when lying on that hip or climbing stairs. The pain often shoots down the outer thigh, making people think they have a hip joint problem when the bursa is actually the culprit.
Repetitive motions trigger most bursitis episodes. Gardening, painting, or even prolonged sitting can inflame these delicate cushions. The pain usually starts gradually, building over days rather than striking suddenly. Ice helps during the acute phase, while gentle movement prevents the joint from stiffening up completely.
Lifestyle Modifications That Reduce Joint Discomfort

Low-impact exercises that strengthen supporting muscles
Swimming and water aerobics top the list for senior-friendly joint exercises. The water’s buoyancy reduces pressure on joints by up to 90% while providing gentle resistance that builds muscle strength. Pool walking, water jogging, and simple arm and leg movements can dramatically improve joint stability without the harsh impact of land-based activities.
Yoga and tai chi offer excellent alternatives for building strength while improving flexibility and balance. These practices focus on controlled movements that strengthen the muscles surrounding joints, particularly in the hips, knees, and spine. Chair yoga modifications make these exercises accessible even for those with limited mobility.
Resistance band exercises provide targeted muscle strengthening without heavy weights. These versatile tools allow seniors to work on specific muscle groups that support problem joints. Simple bicep curls, leg extensions, and shoulder rotations with resistance bands can significantly improve joint function over time.
Weight management strategies for reduced joint pressure
Every pound of body weight translates to approximately four pounds of pressure on weight-bearing joints like knees and hips. Losing just 10 pounds can reduce knee pressure by 40 pounds with each step, making a substantial difference in daily comfort levels.
Effective Weight Management Approaches:
| Strategy | Benefits | Implementation Tips |
| Portion Control | Reduces caloric intake without eliminating foods | Use smaller plates, measure portions initially |
| Meal Timing | Improves metabolism and energy levels | Eat regular meals, avoid late-night snacking |
| Hydration Focus | Reduces false hunger signals | Drink water before meals, aim for 8 glasses daily |
| Food Tracking | Increases awareness of eating patterns | Use apps or journals to monitor intake |
Gradual weight loss of 1-2 pounds per week proves most sustainable and joint-friendly. Crash diets often lead to muscle loss, which weakens the very support system joints need most.
Anti-inflammatory dietary choices that fight pain
Omega-3 fatty acids found in salmon, sardines, and walnuts actively reduce inflammation markers in the body. Aim for two servings of fatty fish per week or consider high-quality fish oil supplements after consulting with healthcare providers.
The Mediterranean diet pattern consistently shows anti-inflammatory benefits. This approach emphasizes:
- Colorful vegetables and fruits: Berries, leafy greens, and bell peppers contain antioxidants that combat inflammatory processes
- Whole grains: Brown rice, quinoa, and oats provide fiber and nutrients while avoiding inflammatory refined sugars
- Healthy fats: Olive oil, avocados, and nuts support joint health and overall inflammation reduction
- Lean proteins: Fish, poultry, and legumes provide building blocks for muscle maintenance
Spices like turmeric, ginger, and cinnamon contain natural anti-inflammatory compounds. Adding these to daily meals can provide cumulative benefits over time. Turmeric, particularly when combined with black pepper, shows promising results for joint pain relief.
Sleep optimization techniques for better recovery
Quality sleep directly impacts pain perception and inflammation levels. During deep sleep, the body repairs damaged tissues and reduces inflammatory markers that contribute to joint discomfort.
Sleep Environment Improvements:
- Keep bedrooms between 65-68°F for optimal rest
- Use blackout curtains or eye masks to eliminate light disruption
- Invest in supportive pillows that maintain proper neck and spine alignment
- Consider memory foam mattress toppers for pressure point relief
Sleep positioning matters significantly for joint health. Side sleepers should place pillows between their knees to reduce hip and lower back strain. Back sleepers benefit from pillows under their knees to maintain natural spine curves.
Establishing consistent bedtime routines helps regulate sleep cycles. This might include gentle stretching, reading, or listening to calming music. Avoiding screens for at least an hour before bed prevents blue light from disrupting natural melatonin production.
Stress reduction methods that minimize inflammation
Chronic stress triggers cortisol release, which increases inflammation throughout the body and amplifies pain perception. Managing stress becomes particularly important for seniors dealing with joint issues.
Deep breathing exercises provide immediate stress relief and can be practiced anywhere. The 4-7-8 technique involves inhaling for 4 counts, holding for 7, and exhaling for 8. This simple practice activates the body’s relaxation response and reduces stress hormones.
Meditation apps designed for beginners make starting a mindfulness practice accessible. Even 10 minutes of daily meditation can significantly reduce stress levels and improve pain management. Guided meditations specifically for chronic pain offer targeted approaches for joint discomfort.
Social connections play a vital role in stress management. Regular contact with friends, family, or support groups provides emotional support that reduces stress-related inflammation. Community activities, volunteer work, or joining senior centers create opportunities for meaningful social interaction while staying physically active.
Medical Treatment Options for Effective Pain Relief

Over-the-counter medications and proper dosage guidelines
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, and aspirin serve as the first line of defense against joint pain for many seniors. These medications tackle both pain and inflammation, making them particularly effective for arthritis-related discomfort. Ibuprofen typically works well at 200-400mg every 6-8 hours, while naproxen offers longer-lasting relief at 220mg twice daily.
Acetaminophen presents another solid option, especially for seniors who can’t tolerate NSAIDs due to stomach issues or blood thinning medications. The standard dose ranges from 325-650mg every 4-6 hours, with a maximum daily limit of 3,000mg for older adults.
Topical pain relievers deserve serious consideration for localized joint pain. Creams and gels containing menthol, capsaicin, or topical NSAIDs like diclofenac can provide targeted relief without the systemic side effects of oral medications. These work particularly well for knee, hand, and elbow pain.
Safety becomes paramount when seniors use over-the-counter medications regularly. NSAIDs can increase bleeding risk, affect kidney function, and raise blood pressure. Anyone taking blood thinners should consult their doctor before using these medications. Acetaminophen, while gentler on the stomach, can damage the liver when combined with alcohol or taken in excessive doses.
Prescription treatments for severe joint conditions
When over-the-counter options fall short, prescription medications offer more powerful pain management strategies. Disease-modifying antirheumatic drugs (DMARDs) like methotrexate and sulfasalazine can slow the progression of rheumatoid arthritis while reducing inflammation and joint damage.
Biologic medications represent a breakthrough for severe inflammatory conditions. These targeted therapies, including adalimumab and etanercept, block specific immune system proteins that cause inflammation. While highly effective, they require careful monitoring due to their impact on the immune system.
Corticosteroid injections provide direct relief for severely inflamed joints. These shots can offer weeks or months of pain relief, though they’re typically limited to 3-4 times per year to prevent joint damage. Hyaluronic acid injections, particularly for knee osteoarthritis, can improve joint lubrication and reduce pain for several months.
Prescription topical treatments like capsaicin patches or compound creams mixed by specialized pharmacies can deliver targeted relief without systemic effects. These work especially well when multiple joints need treatment or when oral medications cause unwanted side effects.
Physical therapy benefits and exercise protocols
Physical therapy stands as one of the most effective non-pharmaceutical treatments for joint pain. A skilled physical therapist can identify movement patterns that worsen pain and teach proper body mechanics to reduce joint stress. They also assess muscle imbalances and weakness that contribute to joint problems.
Range-of-motion exercises form the foundation of most therapy programs. These gentle movements help maintain joint flexibility and prevent stiffness that often worsens with inactivity. Simple exercises like shoulder rolls, ankle circles, and gentle neck stretches can be performed daily at home.
Strengthening exercises target the muscles surrounding affected joints, providing better support and stability. Water-based exercises offer particular benefits for seniors, as the buoyancy reduces joint stress while providing resistance for muscle strengthening. Swimming, water walking, and pool-based aerobics can significantly improve joint function.
Low-impact aerobic activities like walking, cycling, and elliptical training improve circulation, reduce inflammation, and strengthen the heart without excessive joint stress. Starting with 10-15 minutes daily and gradually increasing duration helps build endurance safely.
Balance and proprioception training becomes increasingly important as joint pain can affect stability. Simple exercises like standing on one foot or walking heel-to-toe help prevent falls while improving joint awareness and control.
Natural Remedies That Complement Traditional Treatments

Heat and Cold Therapy Application Techniques
Switching between heat and cold treatments can work wonders for joint pain relief. Heat therapy helps relax stiff muscles and increases blood flow to painful areas, while cold therapy reduces inflammation and numbs sharp pain sensations.
For heat therapy, try warm baths with Epsom salts for 15-20 minutes, or apply heating pads on low settings for no more than 20 minutes at a time. Warm, damp towels work great too – just microwave a damp towel for 1-2 minutes and test the temperature before applying. Never use heat on swollen or inflamed joints, as this can make swelling worse.
Cold therapy works best for acute pain flare-ups. Ice packs wrapped in thin towels should be applied for 10-15 minutes several times daily. Frozen vegetable bags make excellent flexible ice packs that conform to joint shapes. Some people find alternating between hot and cold treatments particularly effective – try 3 minutes of heat followed by 1 minute of cold, repeating this cycle 3-4 times.
Beneficial Supplements for Joint Health Support
Several supplements show promise in supporting joint health and reducing pain symptoms. Glucosamine and chondroitin sulfate are among the most researched options, as they help maintain cartilage structure and may slow joint deterioration.
| Supplement | Daily Dosage | Primary Benefits |
| Glucosamine | 1,500mg | Supports cartilage repair |
| Chondroitin | 800-1,200mg | Reduces joint inflammation |
| Omega-3 fatty acids | 2-3g | Anti-inflammatory effects |
| Turmeric (curcumin) | 500-1,000mg | Natural pain reliever |
| Vitamin D | 1,000-2,000 IU | Supports bone health |
Omega-3 fatty acids from fish oil can significantly reduce joint stiffness and pain intensity. Turmeric contains curcumin, a powerful anti-inflammatory compound that many seniors find helpful for managing arthritis symptoms. Always consult your doctor before starting new supplements, especially if you take blood thinners or other medications.
Massage and Acupuncture Pain Relief Benefits
Regular massage therapy can provide substantial relief from joint pain and stiffness. Gentle Swedish massage improves circulation and helps relax tight muscles around affected joints. Deep tissue massage may be too intense for some seniors, so communicate your comfort level with your massage therapist.
Self-massage techniques can be practiced daily at home. Use circular motions with gentle pressure around painful joints, or try rolling a tennis ball under your feet for plantar fasciitis relief. Massage oils infused with peppermint or eucalyptus can enhance the pain-relieving effects.
Acupuncture has gained recognition as an effective complementary treatment for joint pain. Many seniors report reduced pain levels and improved mobility after regular acupuncture sessions. The treatment stimulates specific points on the body, potentially triggering the release of natural pain-relieving endorphins. Most people need 6-8 sessions to notice significant improvements, though some experience relief after just a few treatments.
Topical Treatments That Provide Targeted Relief
Topical pain relievers offer targeted relief without the systemic side effects of oral medications. These treatments work directly at the pain site and can be particularly effective for surface-level joint discomfort.
Over-the-counter creams containing menthol, camphor, or capsaicin provide cooling or warming sensations that can distract from pain signals. Capsaicin cream, derived from chili peppers, may initially cause mild burning but often provides lasting relief with consistent use.
Topical NSAIDs like diclofenac gel deliver anti-inflammatory medication directly to affected joints with minimal absorption into the bloodstream. This makes them safer options for seniors who cannot tolerate oral pain medications due to stomach issues or other health concerns.
Arnica gel, derived from a mountain flower, is popular among those seeking natural topical relief. While scientific evidence is limited, many people find it helpful for reducing bruising and minor joint discomfort. Essential oil blends containing wintergreen, peppermint, or lavender can be diluted with carrier oils for homemade topical treatments.
Remember to test any new topical treatment on a small skin area first to check for allergic reactions or sensitivity.
When to Seek Professional Medical Intervention

Warning signs that require immediate attention
Joint pain becomes a medical emergency when certain red flags appear. Sudden onset of severe pain accompanied by fever, chills, or sweating suggests possible infection and needs immediate evaluation. If joint pain develops alongside difficulty breathing, chest pain, or rapid heartbeat, these symptoms could indicate a serious inflammatory condition affecting multiple body systems.
Swelling that occurs rapidly over hours rather than days warrants urgent attention, especially when the affected joint feels hot to the touch or appears red and inflamed. Joint deformity, complete inability to move the joint, or joints that feel unstable and give way during normal activities signal potentially serious structural damage.
Seniors should head to the emergency room if joint pain starts after a fall or injury and they cannot bear weight on the affected limb. Numbness, tingling, or color changes in fingers or toes alongside joint pain might indicate compromised blood flow or nerve damage requiring prompt intervention.
Diagnostic tests that identify underlying conditions
Healthcare providers use several diagnostic tools to pinpoint the exact cause of joint pain in seniors. Blood tests reveal inflammatory markers like C-reactive protein and erythrocyte sedimentation rate, which help distinguish between different types of arthritis. Rheumatoid factor and anti-CCP antibodies specifically identify rheumatoid arthritis, while uric acid levels diagnose gout.
X-rays remain the first-line imaging test, showing bone changes, joint space narrowing, and cartilage loss typical of osteoarthritis. MRI scans provide detailed images of soft tissues, revealing ligament tears, meniscus damage, and early cartilage changes not visible on X-rays.
| Test Type | What It Reveals | Best For |
| Blood Tests | Inflammation, autoimmune markers | RA, gout, infections |
| X-rays | Bone structure, joint spacing | Osteoarthritis, fractures |
| MRI | Soft tissue detail | Cartilage, ligaments, early changes |
| Ultrasound | Real-time joint movement | Fluid buildup, tendon issues |
| Bone Scan | Metabolic bone activity | Stress fractures, bone infections |
Joint fluid analysis through arthrocentesis helps diagnose infections, crystal arthropathies like gout, and distinguishes between different inflammatory conditions. This procedure involves drawing fluid directly from the affected joint using a needle.
Specialist referrals for advanced treatment options
Primary care physicians typically refer seniors to rheumatologists when blood tests suggest autoimmune conditions like rheumatoid arthritis or lupus. These specialists manage complex medication regimens including disease-modifying antirheumatic drugs (DMARDs) and biologics that target specific inflammatory pathways.
Orthopedic surgeons become necessary when conservative treatments fail and joint damage significantly impairs daily activities. They evaluate candidates for joint replacement surgery, arthroscopy, and other surgical interventions. Sports medicine specialists focus on injuries and mechanical problems, offering treatments like platelet-rich plasma injections and advanced physical therapy techniques.
Pain management specialists help seniors whose joint pain doesn’t respond adequately to standard treatments. They provide nerve blocks, epidural injections, and coordinate comprehensive pain management plans combining medications, procedures, and psychological support.
Physical medicine and rehabilitation (PM&R) doctors specialize in restoring function and managing chronic pain through non-surgical approaches. They coordinate care between different healthcare providers and focus on improving quality of life through adaptive techniques and assistive devices.
Getting the right specialist referral often depends on the suspected underlying condition and the senior’s overall health status and treatment goals.

Joint pain doesn’t have to define your golden years. While aging naturally brings changes to our bodies, understanding the root causes of joint discomfort and the various treatment approaches available can make a real difference in your daily life. From simple lifestyle adjustments like staying active and maintaining a healthy weight to exploring medical treatments and natural remedies, you have multiple tools at your disposal to manage pain effectively.
The key is finding the right combination that works for your specific situation. Don’t wait until the pain becomes unbearable – early intervention often leads to better outcomes. Talk to your healthcare provider about developing a comprehensive pain management plan that fits your lifestyle and health goals. Remember, staying informed and proactive about your joint health can help you maintain the active, fulfilling life you deserve.